Treating the war-wounded

Contents
23 septembre : création par Colbert, ministre de Louis XIV, de la caisse des invalides de la marine royale.
Ouverture de la Cité des vétérans de l’armée royale, fondée par Louis XIV pour recueillir les soldats blessés, les convalescents et les invalides (renommée en 1792 Hôtel national des militaires invalides).
2 août : loi fixant les retraites et le sort des invalides, érigeant le principe de la réparation en "dette de reconnaissance de la Nation" mais, faute de budget, restant essentiellement une dette morale et symbolique.
16 mai : première loi allouant, sous réserve budgétaire, une pension aux veuves de guerre.
9 mars : décret accordant une bourse aux orphelins indigents y compris enfants de soldats morts pour la patrie.
4 mai : loi accordant des secours aux familles des défenseurs de la patrie.
4 juin : loi relative au droit à pension des veuves de militaires morts aux combats ou par suite de blessures.
6 juin : décret accordant des pensions aux militaires blessés au combat.
1814 : les Invalides rebaptisés "hôtel royal des Invalides".
11 et 18 avril : lois pour la mise en place de procédures au sein de l’institution militaire permettant d’attribuer des pensions aux blessés graves et infirmes incurables victimes "d’événements de guerre" ou d’accidents survenus en service commandé (11 avril pour l’armée de terre, 18 avril pour la marine).
24 juin : acte fondateur de la Croix-Rouge à Solferino par Henry Dunant, témoin de la bataille, improvisant, avec le concours des populations civiles locales, des secours aux soldats des deux camps sans discrimination.
Création du Comité international et permanent de secours aux blessés militaires.
25 mai : constitution de la Croix-Rouge française sous le nom de Société de secours aux blessés militaires (SSBM).
22 août : adoption de la première Convention de Genève pour l’amélioration du sort des blessés et des malades.
31 octobre : fondation de l’Association des dames françaises pour les secours aux blessés militaires (ADF).
Fondation de l’Union des femmes de France (UFF).
6 juillet : deuxième Convention de Genève pour l'amélioration du sort des blessés et malades dans les armées en campagne.
2 mars : création d’un organisme public : l’Office national des mutilés et réformés de la guerre (ONMRG).
27 juillet : loi instaurant le statut de pupille de la Nation et créant un Office national des pupilles de la Nation (ONPN).
2 janvier : création de l’Institut national des Invalides, réaffirmant la double mission d’hébergement et de soins de l’hôtel des Invalides.
31 mars : loi Lugol ouvrant droit à pension aux militaires des armées de terre et de mer affectés d’infirmités résultant de la guerre, aux veuves, aux orphelins et aux ascendants de ceux qui sont morts pour la France.
24 juin : droit à réparation financière étendu aux victimes civiles de la guerre et à leurs ayants cause.
23 janvier : création du ministère des pensions, primes et allocations de guerre.
27 juillet : Convention de Genève relative au traitement des prisonniers de guerre, y compris blessés.
19 avril : l’ONMRG renommé Office national des mutilés, combattants, victimes de la guerre et pupilles de la Nation (ONMCVGPN) après fusion avec l’ONPN.
Création officielle de l’association "Bleuet de France", héritière des ateliers de confection du bleuet constitués en 1925 pour les pensionnaires des Invalides.
Le ministère des pensions renommé ministère des anciens combattants.
7 août : fusion de la SSBM, de l'ADF et de l'UFF pour former une Croix-Rouge française unique.
17 juin : l’ONMCVGPN renommé Office national des anciens combattants et victimes de guerre en intégrant le soutien aux prisonniers, déportés et réfugiés.
6 août : loi relative à la codification des textes législatifs concernant les pensions militaires d’invalidité, les diverses pensions d’invalidité soumises à un régime analogue et les avantages accordés aux bénéficiaires desdites pensions.
12 août : signature de quatre conventions :
- Convention de Genève pour l’amélioration du sort des blessés et des malades dans les forces armées en campagne ;
- Convention de Genève pour l’amélioration du sort des blessés, des malades et des naufragés des forces armées sur mer ;
- Convention de Genève relative au traitement des prisonniers de guerre ;
- Convention de Genève relative à la protection des personnes civiles en temps de guerre.
28 avril : entrée en vigueur du Code des pensions militaires d'invalidité et des victimes de la guerre.
12 novembre : loi allouant un secours annuel égal à la pension de veuve de guerre aux compagnes de militaires, marins ou civils "Morts pour la France".
9 septembre : création d'un Fonds de Garantie chargé notamment de la réparation intégrale des dommages corporels résultant des actes de terrorisme et autres infractions.
23 janvier : loi étendant les "dispositions du code des pensions militaires d'invalidité et des victimes de guerre applicables aux victimes civiles de guerre" aux victimes d'actes de terrorisme.
31 octobre : l’Œuvre nationale du Bleuet de France, faisant suite à l’association Bleuet de France, intégrée à l’ONACVG ; les victimes de terrorisme dès lors ressortissants de l’ONACVG.
30 janvier : l’Institution nationale des Invalides constituée en établissement public à caractère administratif.
28 décembre : refonte de la partie législative du Code des pensions militaires d'invalidité et des victimes de guerre tenant compte des évolutions législatives en vigueur.

Summary
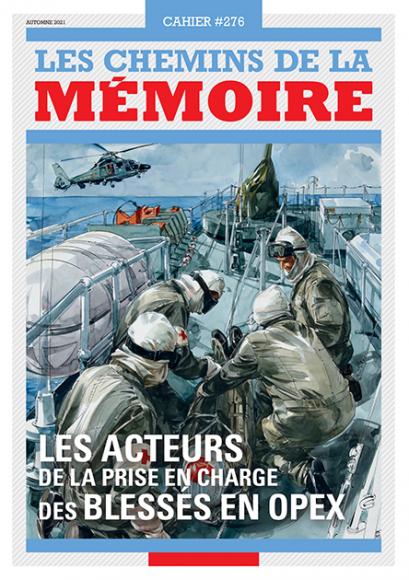
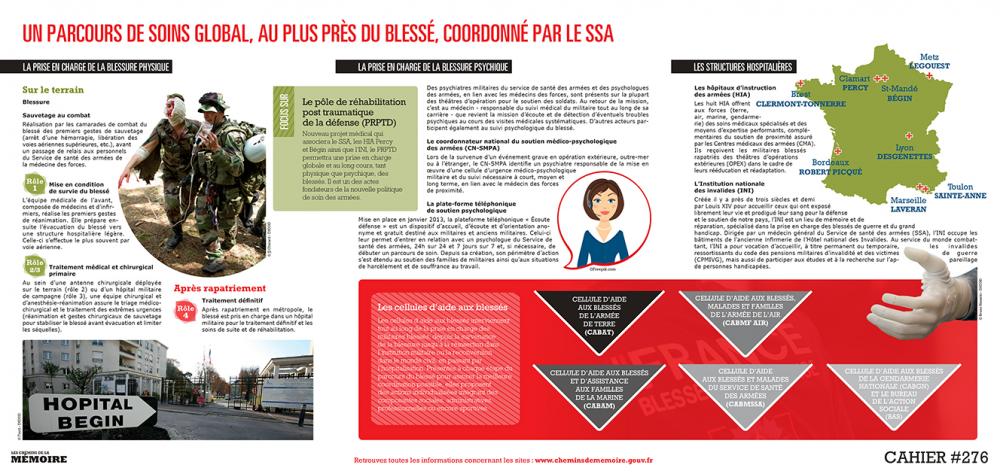
SUBJECT: Military medicine
MISSION: Treating physical and mental trauma
PARTIES INVOLVED: Army health service, army hospitals, army medics
How the wounded are treated on the battlefield since the Franco-Prussian war in 1870 to the most recent interventions has changed extensively, both from an organisational perspective to the ways in which treatment, and what treatment, is administered by health care specialists in the army. In this sense, it has increased the chances of survival of each and every soldier.
By the end of the Franco-Prussian war, in 1871, the final toll of deaths and casualties among the French troops was almost the same between the number of war-wounded (130,000), the number killed (140,000) and those who died from disease (about 300,000, illness and frostbite combined). The huge defeat and toll sounded the death knell on the treatments administered to the war-wounded until then.
The health service, reliant both on the leadership and the supply corps, was in fact not yet considered a service in its own right. As such, the battlefield was a hotchpotch of army medical corps units, aid societies under the authority of the Red Cross and hospitals further into the country. While the principle of rapid evacuation of the war-wounded was advocated by some medical staff, backed by lessons learned during the American Civil War and the Crimean War, how combat played out determined whether this would be possible or not. Under direct enemy threat, the primary caregivers were in danger of being killed or captured such as happened during the retreat to Metz or the Battle of Saint-Privat. Indeed, up until the surrender of Sedan, the doctors stayed on the ground, doing whatever they could to dress the war-wounded lying on the battlefield, becoming as much targets as the troops themselves.
The difficult birth of an autonomous health service post 1870
Treatment administered to the war-wounded was long thwarted by the problems of fighting infection along with the dearth of sterilised bandages, antisepsis during operations as well as morphine, in the army medic’s bag. But the medical world was above all pointing out, until the end of the 19th century, the failings of logistics and links between the different parts of the chain. The Société de Secours aux Blessés Mlitaires, the original name of the French Red Cross, spent months roaming about in 1870, unable to provide the services it was there to, due to a lack of clear orders from the leadership or the supply corps.
Upon the signing of the Treaty of Frankfurt that formalised France’s defeat, on 10 May 1871, a reorganisation of the French army and its health service became a necessity. Drawing lessons from the tragic events of the conflict, the French Academy of Medicine recommended in 1873 establishing an independent health service, which was enshrined by the law of March 1882 and completed by the law of 1 July 1889. Management of the health service was assigned to the medical corps, both in wartime and peacetime, and the medical training was entrusted to the medical authorities.

Temporary first-aid post set up by the Red Cross during the Battle of the Somme, 1916. © TopFoto / Roger-Viollet
Lessons from World War I
The Franco-Prussian war and more recently the French medical interventions during the First Balkan War (1912-1913) provided inspiration to the medical profession. Before the start of WWI, the primary caregivers were obliged to provide emergency care by ‘wrapping up’ the injured before evacuating them away from the front to sites where surgeons could carry out operations. Matters changed when the conflict broke out in 1914.
Following the new wave of violent combat that occurred, surgical ambulances were stationed as close as possible to the battlefield, from around September or October, to start treating the war-wounded as quickly as possible. The health service was run in a rather makeshift way in the first weeks of war as nothing had prepared the medical staff for the onslaught of casualties and dead coming in or the gravity of the physical injuries. The speed at which surgery took place was paramount in order to try and stave off infection and haemorrhagic shock. This was the intention behind the rather controversial amputation technique, known as the ‘sliced sausage’ method, practised by French surgeon Victor Pauchet in the first weeks of war. This consisted of cutting the limb at the point at which the injury occurred. The flesh surrounding the wound was kept and the skin and muscle flaps used to form a solid stump.
The great debacle of 1940
In May-June 1940, the dazzling speed of the advancing German troops during the Battle of France destroyed any organisation already put in place, meaning that the first medical structures set up were unable to function as planned. Various facilities had been installed to accept the war-wounded from the front, such as first-aid posts and advanced surgical units, before they could be evacuated to a hospital away from the front. Scarcely after being provided, the surgical ambulances were forced to pack up and go home. From 15 May, just five days after the start of the German invasion, the entire system planned by the health service was forced back

An injured French soldier being treated, France, 1940. © André Zucca/BHVP/Roger-Viollet
During wartime, the military authorities were responsible for dictating the intervention methods and protocols for medical staff, the conditions for removing bodies and the first-aid to administer in the immediacy of the battlefield. The lightening speed of the German invasion was one reason that led to the dislocation of the French army and its health service.
The health service became part of the general sense of confusion that pervaded the war, depicted for instance by the image of medical vehicles depositing the war-wounded wherever they could when driving away from the front. Overwhelmed by these events, the health service executive often had to leave it to individuals taking their own initiatives, like the case of one doctor working from a hospital in Zuydcoote, in the north of France, which had received over 4,000 war-wounded including 600 brought in on 2 June 1940 alone, and who resolved to stay put while awaiting the arrival of German troops.
The health service’s efforts during the wars of national liberation
The themes of makeshift organisation and difficulty leaving the combat zone were repeated during the Indochina and Algerian wars, as if any ‘lessons’ learned during earlier conflicts had simply been forgotten.
When the French Expeditionary Force landed in Indochina in 1946-1947, the health service was extremely low on resources, which meant that they struggled to transport the wounded to the surgical units in Saigon or Hanoi. As was the case during WWI, the main concern was the need to evacuate victims as soon as possible to start treatment just as quickly.
But until the end of the conflict, the humble stretcher was the primary form of evacuation to transfer injured soldiers to the battalion’s first-aid post or the medical vehicle’s collection point. An exhausting operation for the carriers, forced to plod through jungle or paddy fields, and dangerous for the wounded whose pain and injury were only aggravated during transfer. A perilous mission too for the party protecting the carriers. Rigid stretchers were gradually replaced by lightweight folding stretchers made of aluminium, although hammocks and fishing nets were also commonly employed.

War-wounded evacuated during the Indochina War, 1954. © Roger-Viollet
The major innovation in terms of evacuation technology was the use of aviation from the early 1950s when conflicts became more and more international. This allowed the injured to be evacuated from a combat zone by air and be transported to proper hospitals, where they could be operated on. Widely used by the American military during the Korean War, helicopters appeared in the skies above Indochina around 1949-1950. This mode of transport radically altered the primary evacuations made and the recovery of the wounded from hard-to-reach sites. The helicopter provided a useful aid to medical staff, offering an alternative to the exhausting, long and dangerous carrying of stretchers. However, from what we can make out from the images, evacuations of the wounded using this type of transport was a rare and exceptional occurrence due to the difficult terrain.
In Algeria, the combat methods employed, involving disrupting and attacking remote army posts, in addition to the extreme geographic conditions (steep mountains, sites hard to access) made it very difficult for the primary medics to go about their work and evacuate the war-wounded. The use of air evacuation with a broader range of aircraft including heavyweight Sikorsky helicopters to more lightweight helicopters facilitating the work of the stretcher services to the first-aid post also made it possible to perform an initial triage as well as more remote evacuations. A wounded person could be under the surgeon’s knife one to six hours after being injured.
On the ground, it was the nurse’s job to treat the wounded by performing first aid. The battalion medic would be working from an infirmary often set up in a prefab structure. The conditions were extremely basic but the surgical units did not experience the same development as seen during previous conflicts since there were already facilities for the war-wounded in local hospitals or in towns and cities such as Algiers, Blida, Médéa, Oran, Tlemcen, Constantine, Sétif and Philippeville.
Recent developments
France’s engagement in Afghanistan prompted the health service operating from the battlefield to further hone its specialisation. Treatment was given at different points: medicalisation on the front at the first-aid post, surgical specialisation on the front at the surgical unit and medical evacuations by air as soon as possible.
The introduction of a medical data collection register today allows us to study the medical treatment administered to the war-wounded on the different ranges of trauma observed, the cause of death at every step leading to questions regarding whether any deaths were ‘avoidable’. This line of thinking is a continuation of the research carried out in the US in the seventies. At the time, the surgeon Maughon had examined the autopsy results of 2,600 American soldiers who died in Vietnam, motivated by the idea that they might be able to do more on the battlefield to prevent death, in particular following bleeding out. By analysing the causes of death of casualties on the battlefield, they thought they might be able to increase the survival rate of the war-wounded. Other studies carried out during the same war showed that 40% of those killed during combat died bloodless following haemorrhages that could have been more effectively treated in situ. One report concluded that the swift and effective control of haemorrhages was crucial for survival. Similarly, thirty years later, an analysis of autopsies performed on American soldiers who died in Iraq and Afghanistan revealed that about 80% of victims had injuries that would have been survivable, but they died of bleeding out. Among these injuries, about 20% were injuries to the neck, the axillary region and the groin. Death by haemorrhage could occur within minutes following physical injury. Consequently, rapid treatment of any bleeding point became a crucial concern.

On the battlefield, a doctor from the 3rd Marine Infantry Regiment treats an Iraqi soldier with head and arm injuries, 1991.
© Michel Riehl/ECPAD/Défense
These important observations urged the American medical authorities to prioritise research into new haemostatic agents. Given the urgency of the situation, they settled not on the ‘ideal’ agent but the ‘best available’ one, namely HemCon (a bandage that had proven effective for stopping severely bleeding wounds and even severe arterial bleeding) for the American army and QuikClot (a granulate shown to be effective for treating deep vascular wounds) for the navy and marines.
A new doctrine
Besides the work that went into introducing new haemostatic agents, the whole area of ‘damage control’ was put under the microscope. Popularised in the early 1990s, damage control encompasses all of the measures taken to control a situation on or around the battlefield. The initial studies carried out focused on penetrating abdominal traumas, combining visceral and vascular wounds. They demonstrated the different rates of survival depending on the resuscitation methods employed, ranging from an 11% survival rate using a standard surgical approach to 77% when a damage control procedure was applied. This rate shot up to 90% in 2001 by the same medical team. American surgeon Holcomb worked at refining the concept through the approach known as ‘damage control resuscitation’. This consisted of the surgeon performing only the bare minimum of surgical interventions in a very short operating time to stop bleeding and prevent infection. Priority was therefore given to restoring normal physiology rather than anatomical integrity, as reflected in the return to the use of the tourniquet.

Medicalisation in hostile environments training (MEDICHOS) in Lorient. Real-life conditions treating a mass influx of wounded people assembled in a triage
and treatment zone before they can be evacuated.
© R. Connan/DICOD
Modern tourniquets do not aggravate the risk of amputation or permanent disability. The wounded patient themselves, one of their crew or the medic accompanying the combat group are all given first-aid training including how to apply a temporary tourniquet. Employed in combat zones by British and American troops, tactical tourniquets provide fast and more effective control of bleeding than any other techniques and contribute to reducing the fatal consequences of blood loss.
The latter has also been made possible by transfusions performed from the outset of injury. The process consists of first resuscitating the wounded patient using a hypertonic saline solution to restore a pulse or consciousness to then transport the living victim to the first medical facility where other treatments are administered (red blood cells, plasma, platelets, etc.), to control the state of shock. All of the resuscitation procedures developed in recent years in Iraq and Afghanistan explain the extremely high rate of survival in the various epidemiological surveys conducted and among those with facial injuries in particular
A return to ‘normal’ life?
In this sense, the wars in Iraq and Afghanistan brought the soldiers’ extraordinary capacity for survival into relief. The statistics confirmed the trend. The chances of survival on the battlefield during the wars in Iraq and Afghanistan were higher than in any other previous conflict. According to a study by American surgeon Matthew S. Goldberg carried out between March 2003 to January 2007, 90.4% of wounded service people survived compared to 86.5% in Vietnam. The difference between the two rates may seem modest, but when translated into numbers of lives saved, it is phenomenal.
The capacities for survival on the battlefield may evoke a relative sense of invincibility among survivors, in particular those who return home with disabilities. After all, don’t we have the Invictus Games organised for wounded service men and women from every nation? In the games, people who have lost a limb or who have nothing from the torso down compete, moving about just as nimbly as able-bodied athletes.

The French delegation arriving at the Invictus Games opening ceremony. During the third edition, from 23 to 30 September 2017, 30 wounded service men and women, serving and veterans, and civilians from the Ministry of the Armed Forces took part in the competitions in Toronto, Canada. © A. Thomas-Trophime/DICOD
Treatments administered by medics, especially in the time immediately following injury, have given service men and women new hope when their anatomical disabilities would have been fatal in previous conflicts. With the use of highly sophisticated prostheses for limbs and reconstructive surgery for facial trauma, medicine now has a host of tools at its disposal to give wounded service people a functioning body. Thanks to medical advances, they can now live a life almost as ‘normal’ as if the war had not removed a part of their body.
Treatment of the wounded today also encompasses mental trauma. Following on from PTSD (post-traumatic stress disorder) added to the DSM-III (Diagnostic and Statistical Manual, third revision) in 1980, based on various psychiatric disorders observed among Vietnam war vets, TBI (Traumatic Brain Injury) has emerged more recently. TBI refers to brain trauma caused by exposure to explosive blasts from improvised explosive devices (IED). TBI is the signature diagnosis in the British/American medical discourse from operations in Afghanistan and Iraq (OIF/OEF) although it has not completely stamped out PTSD. Based on estimates, between 13% and 17% of service men and women have received this diagnosis. Over 25% of service men and women are diagnosed with a combination of PTSD and TBI. It is worth pointing out that despite the best efforts of the American army in terms of preventing and understanding disorders related to these diagnoses as well as implementing facilities and new procedures designed to reduce the impact of mental disorders, success remains low. Clearly return to civilian life in peacetime is a harsh reality for those who have experienced the violence of war. What also disturbs the historian in all this is the silence of French psychiatrists regarding the matter, both during and after the war in Afghanistan. There is very little material on the French experience in Afghanistan and, more broadly, the most recent international interventions.
Author
Sophie Delaporte - Senior lecturer, qualified to direct research (HDR), UPJV-CHSSC
Read more
Visages de guerre. Les gueules cassées de la Grande Guerre à l’Afghanistan, Sophie Delaporte, Paris, Belin, coll. Contemporaine, 2017.
"Death and injury rates of US Military Personnel in Iraq", MS. Goldberg, Military Medicine, 2010.
Articles of the review
-
The event
"100 ans pour les "Gueules Cassées""
Read more -
The figure
Musée du Service de Santé des Armées
Created during the First World War at the Val-de-Grâce Military Hospital, the Musée du Service de Santé des Armées (MSSA – the armed forces health service museum) presents the history of military medicine. Most importantly, it gives visitors an insight into why and how it was founded and its mission...Read more -
The interview

Luc Aigle, head physician
Treating wounds and saving lives. This is what head physician Luc Aigle did during the multiple field operations he has participated in. Now dean at the Ecole de Lyon, he is training the next generation of army medics.
Read more

